The Operational Effectiveness of the Multidisciplinary Tumor Board of Jose R Reyes Memorial Medical Center, 2021 - 2022
- PJO
- Jun 21, 2025
- 20 min read
Updated: Dec 1, 2025
1 Section of Medical Oncology, Jose R. Reyes Memorial Medical Center, Sta Cruz, Manila
2 Metropolitan Medical Center, Sta Cruz Manila, Philippines
Corresponding author: Melanie Rose Ho Garces-Chua; melanierosegarces@gmail.com
Original Article
Transforming a Conference Proceeding into a Scholarly Research Article: The Case of ONCOLLABORATE
ABSTRACT
Objective: This study evaluated the operational effectiveness of the Jose R Reyes Memorial Medical Center (JRRMMC) Multidisciplinary Tumor Board (MDTB) and its association with clinical outcome symptom relief from treatment start.
Methods: This retrospective cohort study examined medical records of cancer patients undergoing MDTB case evaluation from June 2021 to December 2022. It examined case planning/ proceedings, case presentation and discussions, adherence to guidelines, treatment planning, and outcome monitoring. The study also evaluated the clinical outcome of symptom relief from the start of treatment.
Results: The primary motivations for case presentations were therapeutic planning (90%) and educational value (92%). In 92%, the MDTB had an organizational leader. 14% of the members used technology to share patient data. In 60% of cases, dedicated administrative staff supported the MDTB and were trained and knowledgeable.
Information collection and distribution of protocols were followed in 98% of cases to ensure uniformity and clarity. MDTB meeting procedures were followed in 98%, and 94% implemented meeting and discussion actions, demonstrating strong MDTB standards and recommendations. The meeting used a standard procedure to discuss 94% of patient cases.
The MDTB decision followed clinical diagnosis and treatment guidelines in 98% and 96%, respectively. Diagnostic tests were available in 80% of cases. There was consistent alignment between pre-presentation and post-presentation diagnoses. Recommended treatments showed variation in 42% of cases post-presentation while remaining the same in 58%. Neoadjuvant chemoradiotherapy was the most common modality for locally advanced rectal cancer, at 34% of 50 cases.
The mean time from the initial patient complaint to treatment initiation was 222.7 (sd: 149.5) days. Most patients experience symptom relief within a month, but some may take up to 74 days. The mean time from the first complaint to symptom disappearance was 383.15 (sd: 108.6) days. After reporting symptoms, most patients found relief within a year. Some patients endured 623 days.
Conclusion: The JRRMMC MDTB revealed favorable aspects of MDTB operational effectiveness. Therapeutic planning and educational value drive case presentations, highlighting the board's focus on patient care and professional development. The consistent alignment between pre-presentation and post-presentation diagnoses in all cases and the variation in recommended treatments demonstrate the robustness of the decision-making process while acknowledging the complexity of some cases. Most patients experience symptom relief within a month, proving the treatment works. While the JRRMMC MDTB has relatively solid organizational practices, it could improve the timeline between patient complaints and treatment initiation.
Keywords: Operational effectiveness, Multidisciplinary Tumor Board, symptom relief
INTRODUCTION
Cancer is a complex and challenging disease requiring a multidisciplinary approach to deliver appropriate and effective patient care. Multidisciplinary tumor boards (MDTB) are crucial for effective cancer care.(1,2,3) Despite the increasing use of MDTB in cancer care, there is a lack of evidence on the operational effectiveness of MDTB and its association with the clinical outcome symptom relief from the start of cancer treatment.
The primary objective of this research is to evaluate the operational effectiveness of the MDTB of JRRMMC and its association with surrogate patient outcomes. The study will assess MDTB workflow (decision-making, case review, treatment planning), adherence to best practices during discussions, the link between MDTB participation and patient outcomes (survival, treatment response, time to subsequent treatment), and factors affecting MDTB impact (coordinator, collaboration, member participation, communication, infrastructure).
The proposed study is significant because it will help identify MDTB's strengths and weaknesses and provide insights into how they can be improved to optimize patient outcomes. The study will also contribute to developing evidence-based guidelines for using MDTB in cancer care.
METHODS
This research employed a retrospective cohort approach to assess the operational effectiveness of the MDTB and its association with patient outcomes. The researcher collected data from MDTB document proceedings and medical records, including clinical notes, pathology reports, radiology findings, treatment plans, and follow-up information (See Supplementary Material S1).
The study involved, firstly, the cohort of cancer patients who received care through a multidisciplinary tumor board case review from January 2022 to December 2022. Subsequently, data on the patient's clinical outcomes were collected retrospectively from the medical records. The data included parameters such as overall survival, treatment response, tumor recurrence, time to initiation of recommended treatment, and time to physical recovery. In addition, the researcher also gathered on the patient's exposure to the MDTB, encompassing aspects like evidence-based decision-making, timeliness, streamlined case management, adherence to MDTB to evidence-based guidelines and best practices, multidisciplinary collaboration and communications, supportive infrastructure, treatment planning, outcome monitoring.
The study subjects were the cohort of cancer patients who received care through a multidisciplinary tumor board case review from June 2021 to December 2022. Regarding inclusion criteria, the researcher first considered patients' cases discussed at MDTB from June 2021 to December 2022. Additionally, the inclusion criteria encompassed patients with a confirmed diagnosis of tumors or malignancies, patients with various types of tumors or malignancies (e.g., breast cancer, lung cancer, colorectal cancer) to ensure a diverse sample, patients aged 18 years or older, patients who received treatment recommendations or interventions from the tumor board, and patients treated and managed within the last two years to ensure the availability of relevant data. On the other hand, the exclusion criteria included patients who received their first treatment outside JRRMMC and patients with insufficient medical records that could not provide necessary data for analysis, including follow-up data. The study used the RECIST CRITERIA to evaluate tumor response.4 The researcher took several steps to ensure the accuracy and completeness of the data collected for the retrospective cohort. The researchers utilized standardized data collection forms to ensure consistent and accurate collection of all relevant data. The researcher blinded the data collectors to the study hypothesis to minimize potential bias during data collection. Additionally, the researchers implemented a thorough training program to ensure that data collectors comprehended the study objectives, methods, and the significance of accurate and complete data collection.
The researchers conducted regular quality checks on the collected data to verify its accuracy and completeness. These checks involved scrutinizing a sample of the data for errors or inconsistencies and promptly correcting any identified issues. To further enhance completeness, multiple data sources, such as medical records, pathology reports, and other pertinent sources, were used to capture all relevant information.
RESULTS
Structure and Processes of JRRMMC MDTB
Table 1 presents the outcomes of document review assessing the organizational structure of the MDTB. In 92%, there was a designated organizational leader for the MDTB, indicating high leadership and accountability in the MDTB process. Collaboration within the team demonstrated consistency and positivity across all cases, with 100% affirmative responses to all sub-questions, suggesting high teamwork, cooperation, and a shared vision for patient care among MDTB members.
Table 1 presents the outcomes of document review assessing the organizational structure of the MDTB. In 92%, there was a designated organizational leader for the MDTB, indicating high leadership and accountability in the MDTB process. Collaboration within the team demonstrated consistency and positivity across all cases, with 100% affirmative responses to all sub-questions, suggesting high teamwork, cooperation, and a shared vision for patient care among MDTB members.
TABLE 1 MDTB organizational setup.

The results revealed a low adoption and utilization rate of technology within the MDTB process, with only 14% of cases leveraging technology to facilitate patient information sharing. This low percentage suggests potential barriers, such as lack of availability, accessibility, affordability, user acceptance, or a mismatch between the technology and the needs of MDTB members or the healthcare system itself. However, when technology was employed, it was reliable and secure in all cases, suggesting a high level of quality and trustworthiness in the technological aspects of the MDTB process.
About 60% had dedicated administrative staff supporting the MDTB, who were trained and knowledgeable in 60% of cases, indicating a moderate level of support and capacity for the MDTB process. Nevertheless, this implies that there were instances where the MDTB process lacked sufficient administrative support or expertise, posing potential sources of inefficiency and error. Table 2 shows the outcomes of document review on preparation before MDTB meetings.
TABLE 2 Preparation prior to MDTB.

Outdated patient information was found in 98% of cases, highlighting potential risks to the quality of MDTB decision-making. This finding underscores the critical need for improvements in data collection, management systems, and communication among MDTB members and primary care providers.
Table 3 shows that recommended treatments varied in 42% of cases from pre-presentation while staying the same in 58%.
TABLE 3 Case presentation proceedings.

About 80% of cases had diagnostic tests available during MDTB meetings, demonstrating good planning and collaboration between primary care physicians and MDTB members—however, 68% experienced delays in receiving diagnostic results.
For diagnostic accuracy and completeness, 82% of cases had correct and complete results, and 86% had access to accurate and complete diagnostic reports.
In every case, the post-presentation diagnosis agreed with the pre-presentation diagnosis, suggesting that primary care physicians and MDTB members had a high degree of consensus regarding the patient's status and prognosis. Additionally, 20% observed a change in the recommended diagnostic test, and 42% saw a change in the recommended treatment, indicating that the MDTB conference had a moderate impact on patient management. The MDTB meeting provided a valuable forum for members to exchange viewpoints and knowledge and to update plans considering the most recent research and best practices.
Table 4 shows a high adherence rate of 98% to the defined information collection and distribution protocols. By implementing the protocol, the MDTB process ensures uniformity and clarity. They act as a standardized structure for submitting case protocols, encompassing patient history, physical examination findings, ancillary test results, working impressions, encountered difficulties, and a critical data summary compiled for each patient. They act as a standardized structure for submitting case protocols, encompassing patient history, physical examination findings, ancillary test results, working impressions, encountered difficulties, and a critical data summary compiled for each patient.
TABLE 4 Case discussion proceedings.

TABLE 4 (Continued) Case discussion proceedings.

Following standard operating procedures for case discussions, residents and fellows-in-training submitted cases electronically via email. Prior to the MDTB session, any necessary clarifications were actively sought through email exchanges or personal communication on Viber. During the actual MDTB meeting, presenters employed a standardized format by delivering their cases using PowerPoint presentations.
About 98% of the cases followed these procedures in MDTB meetings, and 94% of the cases implemented the actions from the meeting and discussion, demonstrating strong adherence to MDTB standards and recommendations. Consistency and clarity were ensured throughout presentations by having a single presenter provide all the information for each case. All pertinent members were present in 86% of the cases, which suggests that the MDTB meeting was well- attended and engaged.
In 98% of cases, patient information was manually curated or prepared. In 94%, carefully chosen material was included in the presentation, demonstrating high effort and quality in the data synthesis and preparation process. In 88%, the patient information contained all pertinent information, demonstrating completeness and relevance for the MDTB decision-making process. These results indicate a standardized and well-organized method for case discussions during MDTB meetings.
For 94% of cases, a standardized procedure was in place to discuss patient cases, indicating a high degree of uniformity and structure in the MDTB discussion process. In 76%, a standardized presentation format was utilized, with consistency observed in 70% compared to previous meetings, reflecting moderate variation and flexibility in presentation style. The clarity and comprehensibility of the presentation format were high across all cases, indicating an effective and efficient information transmission and comprehension process.
The process of capturing MDTB discussions followed a set timeline: cases were submitted to medical oncology via email with an off every Friday at 11:59 p.m., the Zoom link and cases received were shared with the MDTB community Viber on Saturday, and the actual discussion occurred on Thursday at 2 p.m. The MDTB implemented a standardized process to capture and document all discussions for every case. This approach demonstrates the team's commitment to high accountability and transparency in the MDTB documentation and reporting process.
The standard process for documenting MDTB discussions involved assigning a main moderator for the week and co-moderators from the presenting service providing the case. During the MDTB session, case presentations and dilemma discussions were followed by clarifications and expert opinions from different departments, concluding with a consensus on the planned management. For 80% of cases, members of the MDTB were aware of the standardized process, indicating a good level of familiarity and knowledge regarding MDTB documentation and reporting procedures. Table 5 shows the results of the document evaluation evaluating the guidelines for implementability and feasibility that were adhered to in MDTB meetings.
TABLE 5 Guideline feasibility.

In 98% of cases, the MDTB decision adhered to clinical recommendations for diagnosis, and in 96%, it followed guidelines for treatment. This high conformance shows that the MDTB decision-making process adheres to best practices and evidence-based standards.
Regarding practicability and viability, the suggested diagnostic procedures could be carried out in 78% of cases, and the recommended course of therapy could be carried out in 86% of cases. These numbers point to a high degree of practicality and applicability of MDTB recommendations in patient care and clinical settings.
There were situations where the suggested diagnostic procedures or therapies could not be carried out or were impossible, suggesting that obstacles may exist to the MDTB implementation and assessment process. These obstacles could result from accessibility, acceptability, price, availability, or suitability of a treatment or diagnostic choice for a patient or the healthcare system.
Association of JRRMMC MDTB with Clinical Outcomes
Eligible 50 patient cases were discussed in the MDTB meetings, and their characteristics are shown in Table 6. Complementing these patient demographics, Table 7 illustrates the distribution of cancer diagnoses based on their intent and treatment modalities. The predominant intent and modality observed were neoadjuvant chemoradiotherapy (ChemoRT; 34%) for locally advanced rectal cancer requiring preoperative intervention to enhance surgical outcomes. The study investigated the application of Neoadjuvant ChemoRT across various cancer stages (II, III, and IV) and subtypes (well-differentiated, poorly differentiated, mucinous).
TABLE 6 Sociodemographic profile (n=50).

TABLE 7 Treatment intent and modalities.
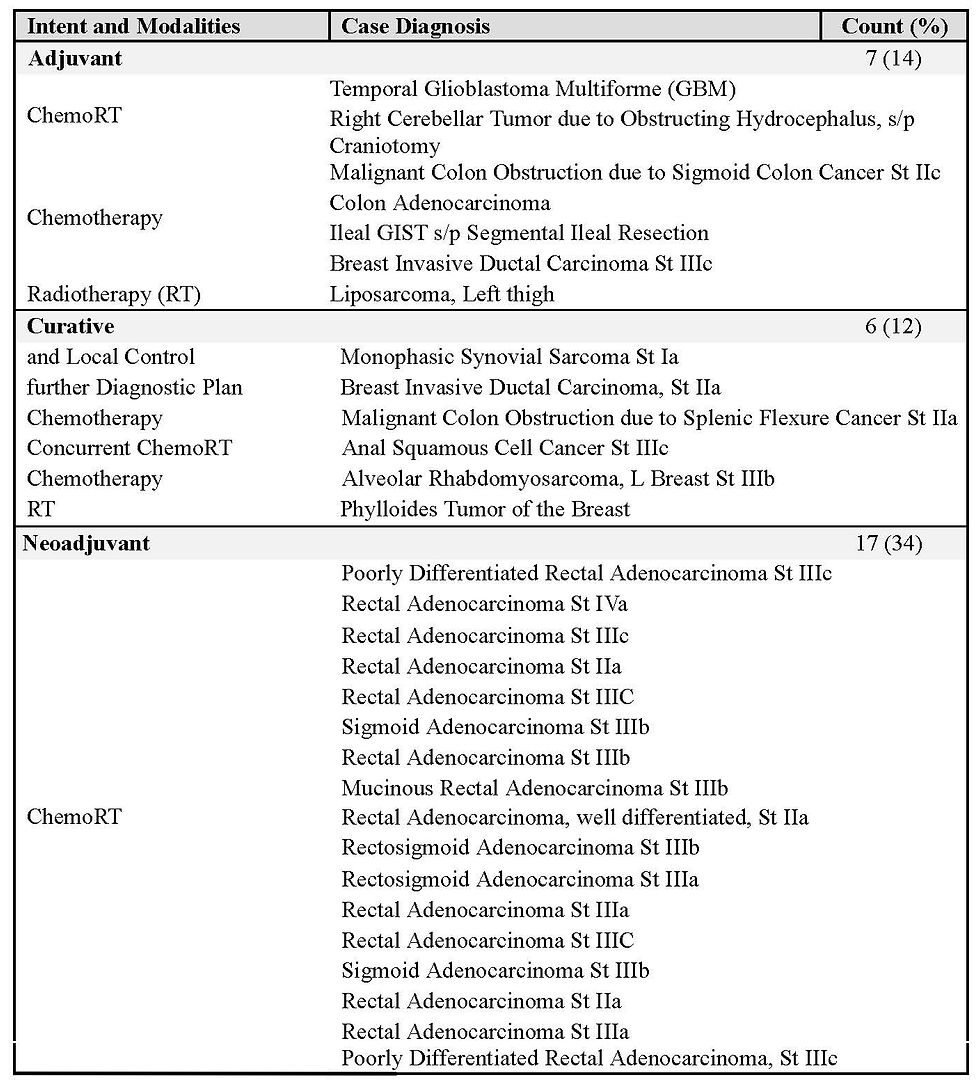
TABLE 7 (Continued) Treatment intent and modalities.

Rectal adenocarcinoma was the most common case (48% of 50 cases).
For the clinical outcome impact of the JRRMMC MBTD, Table 8 shows the duration from the initial recorded patient complaint to the initiation of treatment after MBTD, with a mean of 222.7 (sd: 149.5) days, a median of 172 days, and a mode of 266 days (range 62-682 days) indicating considerable variability. This variance suggests notable delays for certain patients in commencing their treatment.
TABLE 8 Timelines.

The mean duration from treatment initiation to symptom disappearance, or recovery, was moderate at 31.54 (sd: 12.21) days: median 27 days; mode 21 days (range 1-74 days). The mean duration from the first recorded complaint to symptom disappearance was moderate at 383.15 (sd: 108.6) days; median 332.5 days; mode 269 days (range 187-623 days).
DISCUSSION
MDTB Structure and Processes
Document analysis shows commendable MDTB planning and case selection. Tumour board cases match previous treatment, diagnostic, and educational usefulness research.5 However, obsolete patient information threatens MDTB decision-making quality and safety. Addressing this issue and improving decision-making requires strengthening data collecting, administration, and communication systems.
Document assessment identifies strengths and weaknesses in MDTB decision-making. The team must prioritize reducing diagnostic results delays and adapting to therapy adjustments while maintaining diagnostic consistency and accuracy. A delay in the evaluation of test results could delay diagnosis and treatment, resulting in poor clinical outcomes and extended hospital stays.(6) MDTB is a crucial forum for collaborative decision-making and patient management innovation. The document assessment shows that MDTB case discussions are well-organized, consistent, and transparent. The results demonstrate MDTB's dedication to decision-making uniformity, structure, and improvement. MDTB recommendations and clinical adherence are practical. Multidisciplinary tumor boards increase decision-making, clinical adherence, and treatment outcomes.(3) However, the feasibility of implementation highlights the need to continuously evaluate and update guidelines to address real-world restrictions and improve patient outcomes. From the MDTB's organizational perspective, there is strong leadership, excellent collaboration, and precise knowledge of keywords. Despite these characteristics, technology adoption could be faster due to low usage of administrative support and competence variances. Digital tumor board systems help standardize operations, reduce staff workload, and encourage interdisciplinary treatment decision-making, improving patient care.7 By addressing technology use challenges, the team members can improve MDTB efficiency and effectiveness, ultimately guaranteeing excellent patient care and decision-making.
Treatment Time
Interpreting the period between the initial complaint and treatment commencement gives several insights: The extended mean and median durations emphasize the need to improve healthcare system efficiency to treat patients quickly. The vast range of durations implies that the nature and severity of the illness and the patient's access to healthcare contribute to treatment delays. Limited health literacy, distance to treatment locations, and access to care inequalities can delay treatment.8 Standard deviations above the mean indicate a skewed distribution with longer durations more common. The significant proportion of patients with 266 days or less (75%) implies that most patients receive therapy quickly.
According to the data, most patients experience symptom relief within a month of therapy initiation, although others take longer. The following interpretations are possible: The treatment's mean and median durations show significant symptom relief within an acceptable timeframe. The moderate range of recovery times suggests that both a patient's health and the severity of their illness influence the duration of their recovery.
The lower standard deviation than the mean indicates a well-balanced distribution of recovery lengths across the patient population. The 75% of patients who report symptom improvement in 35 days or fewer indicate that most individuals experience symptom alleviation quickly. Different cancer kinds have different treatment initiation times, determining the duration between therapy and symptom decrease. The time to symptom reduction once treatment begins depends on the therapy modalities and the patient's response. As a result, the time it takes from treatment to symptom relief can vary greatly.(9,10)
From the first complaint to symptom absence, most patients see symptom improvement after a month of medication, but others take longer. The following interpretations are possible: The treatment's mean and median durations show significant symptom relief within an acceptable timeframe. The moderate range of durations suggests that the patient's health and the illness's severity affect recovery time. The lower standard deviation than the mean shows a well-balanced recovery length distribution. The 75% of patients who report symptom improvement in 35 days or fewer indicate that most individuals experience symptom alleviation quickly.
Limitations
This investigation has several limitations. Firstly, it relies solely on document review. This approach offers a snapshot of information at a specific point but inherently limits the depth of information available. Crucial real-time interactions that provide insights into the MDTB's efficiency and operational effectiveness might be missing. Secondly, the data used consists of condensed information and summary figures. While these provide a general overview, they may not always capture the full context of a situation. Additionally, prioritizing specific types of cases or documents during selection can introduce bias. Existing documents might lack essential nuances, and overlooking selection bias is a potential pitfall. Thirdly, document reviews offer a static view, potentially missing changes or improvements in MDTB efficiency that have occurred over time. This can lead to a loss of key insights into the evolution of the MDTB process.
Another limitation is the potential for subjective interpretation. Different reviewers may interpret the material differently, introducing bias into the analysis and impacting the study's reliability and validity. Additionally, documents may not contain all pertinent information regarding a case or the MDTB process. Incomplete information can hinder researchers' ability to examine the elements influencing the MDTB's operational effectiveness adequately. The results of a document review may also be specific to the institution or location where the MDTB operates. Generalizing the findings to different contexts or healthcare systems might be difficult, limiting the study's external validity. Furthermore, document evaluations often focus on quantitative data, potentially neglecting valuable qualitative insights. Without in-depth interviews or other qualitative data-gathering methodologies, the viewpoints and experiences of key stakeholders participating in the MDTB may be overlooked.
Moreover, the MDTB's operational effectiveness may change over time since healthcare practices are dynamic. Document reviews may not reflect real-time alterations or adaptations to the MDTB process in response to challenges or criticism. Similarly, if the document evaluation focuses on MDTB technology utilization, it may not fully reflect the user experience or the reasons for technology adoption or non-adoption. Understanding the human factors associated with technology use is crucial for a thorough examination. Finally, document evaluations may lack the context to grasp the reasons for confident MDT choices or actions properly. Drawing reliable conclusions regarding the factors driving efficiency and operational effectiveness can be difficult without contextual information.
Study design and outcome interpretation should consider these limitations carefully to mitigate them. Combining document reviews with other research methods, such as interviews or observations, and ensuring a large, representative sample can strengthen the study's findings.
Implications
Understanding the operational effectiveness of Multidisciplinary Tumor Boards (MDTBs) is critical for optimizing patient care. Efficient MDTBs can lead to faster, more effective treatments through improved decision-making processes within the board.(11) This study goes beyond just identifying strengths and weaknesses; it illuminates the potential for significant improvements across various aspects of cancer care.
Empowering Healthcare Organizations and Policymakers
This research empowers healthcare organizations to implement quality improvement programs, optimize procedures, and foster collaboration across specialties.(12) By identifying factors influencing MDTB efficiency, the study can inform the development of best practices in multidisciplinary cancer care. Sharing these best practices across healthcare institutions can lead to an overall improvement in the quality of cancer treatment.(13)
Furthermore, the findings can inform resource allocation for healthcare managers and policymakers. Understanding the resource needs and challenges of running an efficient MDTB is crucial for ensuring that the right people, technology, and infrastructure are available to support effective multidisciplinary decision-making.(14) This knowledge can guide resource allocation decisions and ensure optimal support for efficient MDTB operations.
Establishing a Foundation for Continuous Improvement
The study also establishes a baseline for ongoing evaluations of MDTB operational effectiveness. Continuous monitoring and improvement are essential in healthcare settings, and this research lays the groundwork for implementing changes and analyzing their impact over time.(15) The data can also inform the development of educational programs and training initiatives for healthcare professionals. Understanding MDTB dynamics can improve interdisciplinary communication and collaboration, benefiting patient outcomes.(16)
Opening Doors for Future Research
Beyond establishing a baseline for MDTB operational effectiveness, this study opens doors for future research endeavors. Here are some promising areas for further exploration:
Longitudinal Studies: Analyzing the long-term impact of efficiency-based modifications on patient outcomes, recurrence rates, and survival rates can assess how advancements in MDTB approaches impact patients over time.(17)
Qualitative Research: In-depth interviews or focus groups can delve into the human element, providing valuable insights into the experiences and perspectives of key stakeholders (healthcare professionals, patients, administrative personnel) and how human factors influence MDTB effectiveness.(16)
Technology Exploration: Studies can explore user experience, identify barriers to technological adoption, and understand how human factors influence the effectiveness of technology within MDTBs.(18)
Comparative Studies: Evaluating MDTB procedures, protocols, and outcomes across institutions can reveal institutional-level factors contributing to efficiency disparities.(19)
Educational Program Effectiveness: Assessing the success of educational programs in enhancing team communication and decision-making can inform the development of tailored interventions.(20)
Patient-Centered Research: Understanding patients' preferences, needs, and experiences can inform strategies to incorporate their perspectives into decision-making, leading to more patient- centered treatment approaches.(20)
Economic and Resource Implications: Calculating resource needs for maintaining optimal efficiency and measuring the cost-effectiveness of improvement initiatives can provide valuable insights for resource allocation.(15)
Cross-Disciplinary Collaboration: Examining the applicability of multidisciplinary approaches to decision-making in other medical fields can broaden our understanding of effective collaboration models across healthcare.(21)
Patient-Reported Outcomes: Integrating patient-reported outcomes into the evaluation process is crucial for understanding how they correlate with clinical assessments and providing a complete picture of treatment success and patient satisfaction within the multidisciplinary care system.(22) This research on MDTB operational effectiveness lays a strong foundation for future advancements. By pursuing these diverse research avenues we can leverage the insights gained from this study to improve MDTB effectiveness continuously. Ultimately, this will lead to better patient care and outcomes.
CONCLUSION
The study on the operational effectiveness of MDTB document review provides essential insights into the mechanisms driving collaborative decision-making in cancer care. The findings highlight the MDTB strengths and possible areas for improvement, laying the groundwork for improving patient outcomes and overall healthcare quality.
The study emphasizes the significance of ongoing research and quality improvement programs in addressing the complexity of transdisciplinary decision-making. While the MDTB is an essential platform for collaborative decision-making, some complexities and limitations necessitate ongoing attention and adaptation.
Furthermore, the study underlines the importance of thoroughly understanding the factors that influence treatment delays and recovery duration. These factors are crucial for customizing interventions that maximize MDTB efficiency, guaranteeing timely and effective patient care.
Future research should include longitudinal investigations, qualitative explorations of stakeholder experiences, and comparative assessments across healthcare facilities. An emphasis on technology adoption, patient-centered research, and the economic consequences of MDTB efficiency improvements will also help to a more comprehensive knowledge of multidisciplinary cancer treatment.
In conclusion, this study is a foundation for future research and improvement efforts in the healthcare system. The goal is to improve MDTB processes, foster collaboration, and improve patient-centered, efficient, and effective cancer treatment delivery.
DATA AVAILABILITY STATEMENTS
Not publicly available.
ETHICS STATEMENT
The Ethics Review Board/Committee of Jose R. Reyes Memorial Medical Center approved the study.
AUTHORS CONTRIBUTION
MRHGC, writing final proposal draft, data curation, writing manuscript
SLB, final conceptualization, approved proposal submission, supervision, review of manuscript SBTJ, initial conceptualization, writing initial proposal draft, methodology, writing manuscript, editing
FUNDING
This research received no external funding.
CONFLICT OF INTEREST
The authors declare no conflicts of interest related to commercial or financial relationships.
PUBLISHER’S NOTE
This article reflects the views and findings of the authors alone and does not necessarily represent the official position of the author's affiliated organizations, the publisher, editors, or reviewers. We encourage readers to remember that the content presented here does not constitute endorsement or approval by any of the entities above.
DECLARATION OF USE OF GENERATIVE ARTIFICIAL INTELLIGENCE
In the preparation of this manuscript, Gemini 1.5 Flash and Grammarly were utilized to refine grammatical structure and phrasing. The authors have thoroughly reviewed, edited, and verified all content generated by AI, taking full responsibility for the accuracy, integrity, and originality of the final published work. The use of AI did not extend to data analysis, interpretation of results, or the drawing of scientific conclusions. All scientific content, intellectual contributions, and research findings presented herein are solely those of the authors.
Similarly, any products or services mentioned within this article are for informational purposes only. The publisher recommends that readers conduct independent evaluations before making any decisions, as the publisher does not guarantee or endorse any products or services mentioned.
REFERENCES
Mano MS, Çitaku FT, Barach P. Implementing multidisciplinary tumor boards in oncology: a narrative review. Future Oncol. 2022 Jan;18(3):375-384.
Rocque G, Wheeler S, Williams GR. The missing voice in multidisciplinary tumor boards. Journal of Geriatric Oncology. 2021 Nov 1;12(8):1157-8.
Cozzolino M, Mannocci A, Carini E, Spina F, Castrini F, Grieco A, et al. The Impact of Tumor Boards on Breast Cancer Care: Evidence from a Systematic Literature Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19(22):14990.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumors: revised RECIST guideline (version 1.1). Eur J Cancer. 2009 Jan;45(2):228-47.
Charara RN, Kreidieh FY, Farhat RA, Al-Feghali KA, Khoury KE, Haydar A, et al. Practice and Impact of Multidisciplinary Tumor Boards on Patient Management: A Prospective Study. J Glob Oncol. 2016 Aug 10;3(3):242-249.
Ong MS, Magrabi F, Coiera E. Delay in reviewing test results prolongs hospital length of stay: a retrospective cohort study. BMC Health Serv Res. 2018 May 16;18(1):369.
Hammer RD, Fowler D, Sheets LR, Siadimas A, Guo C, Prime MS. Digital Tumor Board Solutions Have Significant Impact on Case Preparation. JCO Clin Cancer Inform. 2020 Aug;4:757-768.
Wassie LA, Tsega SS, Melaku MS, Aemro A. Delayed treatment initiation and its associated factors among cancer patients at Northwest Amhara referral hospital oncology units: A cross- sectional study. International Journal of Africa Nursing Sciences. 2023 Jan 1;18:100568.
Chiou SJ, Lin W, Hsieh CJ. Assessment of duration until initial treatment and its determining factors among newly diagnosed oral cancer patients: A population-based retrospective cohort study. Medicine (Baltimore). 2016 Dec;95(50):e5632.
Cone EB, Marchese M, Paciotti M, et al. Assessment of Time-to-Treatment Initiation and Survival in a Cohort of Patients With Common Cancers. JAMA Netw Open. 2020;3(12):e2030072.
Wong BO, Blythe JA, Wu A, Batten JN, Kennedy KM, Kouaho AS, Wren SM. Exploration of Clinician Perspectives on Multidisciplinary Tumor Board Function Beyond Clinical Decision-making. JAMA Oncol. 2022;8(8):1210-1212.
Schellenberger B, Diekmann A, Heuser C, Gambashidze N, Ernstmann N, Ansmann L. Decision-Making in Multidisciplinary Tumor Boards in Breast Cancer Care - An Observational Study. J Multidiscip Healthc. 2021;14:1275-1284.
Kelley S, Beck AC, Weigel RJ, Howe JR, Sugg SL, Lal G. Influence of endocrine multidisciplinary tumor board on patient management and treatment decision making. Am J Surg. 2022;223(1):76-80.
Lamb BW, Green JS, Benn J, Brown KF, Vincent CA, Sevdalis N. Improving decision making in multidisciplinary tumor boards: a prospective longitudinal evaluation of a multicomponent intervention for 1,421 patients. J Am Coll Surg. 2013;217(3):412-20.
Greenhalgh T, Taylor R, Hindmarsh J, Stubbs TL. Studying quality improvement in healthcare. BMJ. 2016;353:i1158.
Arora S, Ashraf I, Davies H, et al. The COMET Initiative: new guidance for developing and evaluating complex interventions. BMJ. 2010;341:c3873.
Steinsapir KD, Galanter JM, Lynch CF, et al. Long-term outcomes of surgery for esophageal cancer: Influence of a multidisciplinary approach. J Thorac Cardiovasc Surg. 2004;128(3):444-52.
Singh H, Mehrotra A, Kalra MK, et al. Adoption and use of electronic health records systems in India: a systematic review. J Healthc Inform Res. 2014;22(2):252-62.
Ovretveit T, Dahm Ø, Glørstad T, et al. Variation in practice and outcome for patients with chronic obstructive pulmonary disease in general practice: a cross-sectional study. BMC Fam Pract. 2014;15:172.
Izzo G, Rocco M, Bifulco A, et al. The role of team training in improving teamwork in surgery: a systematic review. Surg Endosc. 2006;20(2):275-83.
Nutting CM, Goodwin PJ, Harnden P, et al. Randomized trials of breast cancer treatment in older women: a systematic review. J Natl Cancer Inst. 2004;96(8):648-59.
McHorney CA, Kosinski M, Ware JE. Validity and reliability of the SF-36 health status scales. J Clin Epidemiol. 1994;47(3):303-11.
Received: 2023 Dec 12 Received in revised form: 2024 Mar 08 Accepted: 2024 Jun 11
CITATIONS
Garces-Chua MRH, Balete SL, Tanael SB. The operational effectiveness of the multidisciplinary tumor board of Jose R. Reyes Memorial Medical Center, 2021-2022. Philipp J Oncol [Internet]. 2025 [cited 2025 Jun 9];1(1):e009. Available from: [https://www.philsoconc.org/post/the-operational-effectiveness-of-the-multidisciplinary-tumor-board-of-jose-r-reyes-memorial-medical-1]

Comments